After winning the passage of HB1085, which will raise insurance reimbursement rates for therapists, advocates continue to build power to get people with private insurance the care they pay for.
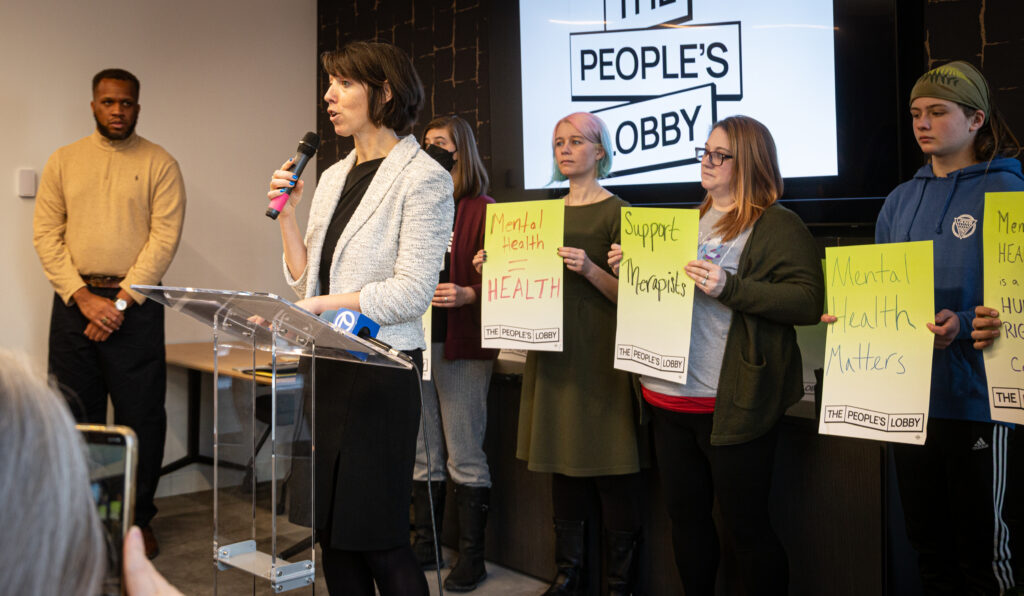
At a press conference on February 9, State Rep. Lindsey LaPointe and State Sen. Karina Villa united with mental health practitioners and patients to force insurance companies to adequately cover mental and behavioral health care.
Last week, Rep. Lindsey LaPointe filed the Preventing Crisis Cost Shifting to Medicaid Act, which would require private insurers to pay their fair share for the mental and behavioral health crisis infrastructure their customers rely on, rather than shifting those costs to Medicaid and other publicly funded systems.
This legislation builds on the momentum that the General Assembly, the People’s Lobby, therapists, patients, and patient advocates built by passing HB1085, also called the Mental Health Parity Law, in October of 2025. Gov. Pritzker signed it into law in December.
For years, Illinois has been suffering under a shortage of therapists. This is due in part to the fact that therapists haven’t received a significant raise from insurers for more than 15 years, forcing many of them to stop accepting insurance, risk burnout by taking on unsustainable caseloads, or leave the profession entirely. Adding insult to injury, insurance corporations have historically forced therapists to sign non-disclosure agreements, making it impossible for them to negotiate for a living wage.
When HB1085 is fully enacted in 2027, it will force private insurers to bring the rate at which they reimburse mental and behavioral health providers more in line with the way physical health practitioners are paid.
“If you or a loved one has ever struggled to find a therapist that accepts your insurance, this is why,” said Allison Staiger, a therapist and a leader with The People’s Lobby. “It’s not just in my best interest as a therapist–it’s in the best interest of my patients that we get together and fight to force these insurance companies to provide the care we pay them to provide.”
When People’s Lobby leader Kristen Holub’s teenage child experienced an acute mental health crisis in 2022, she found that there were no providers available in the network to provide the care they needed. Despite the fact that her family has insurance and her child was already in therapy, she was forced to take her child to the emergency room and then pay out-of-pocket for an out-of-network provider to actually improve her child’s mental health and prescribe the right medications.

“My husband has a good job, and we have “great” insurance, but even with all of that, we could not find the care we needed for my teen. It was just heartbreaking,” Holub said. “I just thought, how on earth would I have handled this if I didn’t have all the resources and support that I did? When you’re already struggling and need mental health care for yourself or a loved one, that’s a terrible time to try to navigate a broken system or advocate for your needs. That’s what led me to join up with The People’s Lobby, so I could fight for people to get the care they need, when they need it.”
“This is about fairness, and it’s about affordability,” said Rep. LaPointe. “Patients and providers joined forces to pass this bill because people shouldn’t have to pay $250 out of pocket for therapy on top of their monthly premiums. We’re showing insurance companies that they can’t just take our money and offload the costs of providing care to taxpayers and individuals. HB1085 was a big step in the right direction last year, and we’ll keep growing access to care this year with the Preventing Crisis Cost Shifting to Medicaid Act.”
“As a school social worker, I personally saw how outdated and inconsistent reimbursement rates pushed behavioral health providers out of insurance networks, leaving families across our state to choose between costly out-of-network care or going without treatment altogether,” said Sen. Villa. “HB 1085 marked a turning point in holding insurance companies accountable. With the Preventing Crisis Cost Shifting to Medicaid Act, we are continuing and strengthening that fight.”
